Health Plans

With rising costs of care and fast-changing regulatory mandates, health plans need to invest in technology solutions that drive value-based care. Hexplora helps overcome various challenges in the areas of risk stratification, population health, accountable care and regulatory challenges like HEDIS and STAR.
Hexplora’s Benefits for Health Plans

Drive Value-Based Care

Elevate Member’s Experience

Problem-free Provider Network Management

Track Health Care Performance
All-inclusive analytics suite for Health Plans to go beyond the limits

Elevate member's experience
Offer top-notch services to members by improving engagement at every step, accelerating gap closure, sharing proactive measures over symptoms. Doing so will empower your enrollees to be your brand advocate and improve members' retention. With Hexplora's comprehensive analytics platform, any growing health plans can unleash performance with actionable insights transforming patient care.
Achieve Top NCQA rating across all measures
Being officially HEDIS certified, Hexplora is a trusted advisor for health plans on the accuracy of quality measure rates and care gaps. Our experts work hand-in-hand with health plans to ensure integrity and engage providers in compliance with quality measures. Our quality reporting solution allows health plans to track performance measurement of Quality Measures across Commercial, Medicare, and Medicaid lines of business, including HEDIS, STARs, and state-specific Medicaid measures.

Problem-free Provider network management
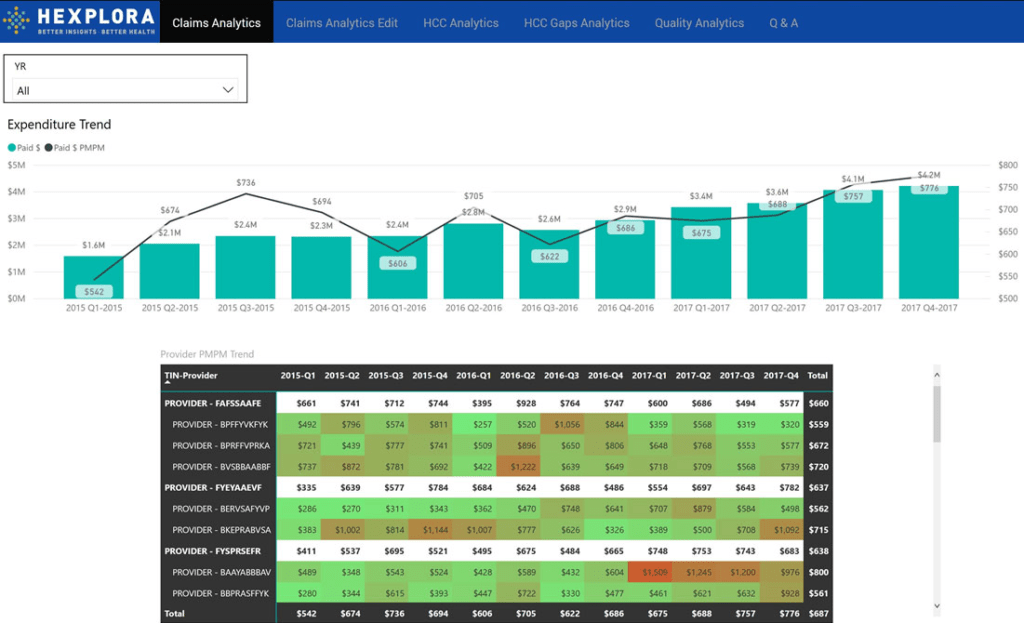
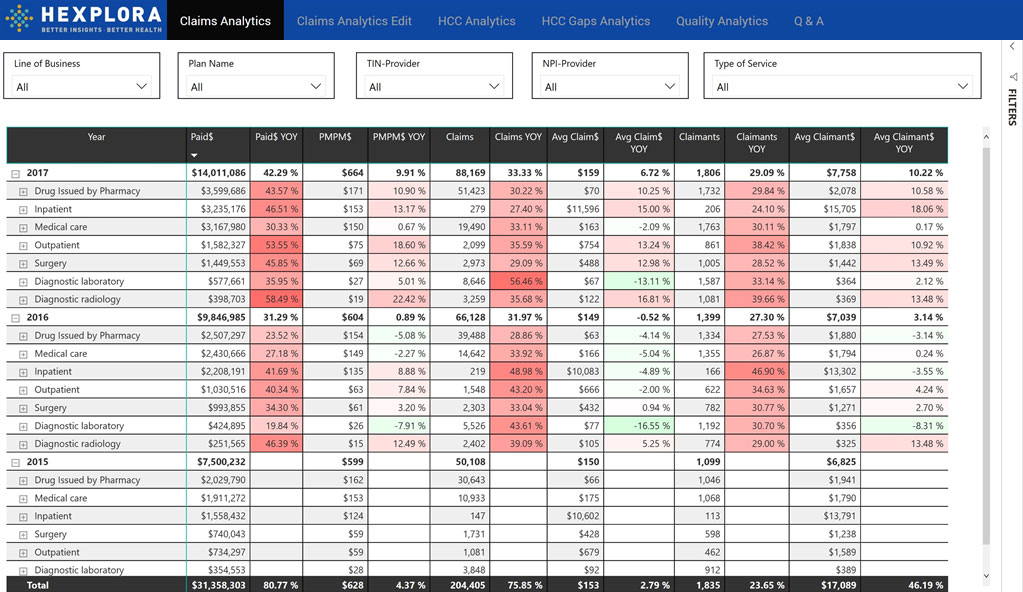
Have you noticed that many health plans have fallen into steep decline? One of the principal causes of poor members' experience is the collaboration gap with providers. Improving the collaboration and engagement will significantly improve desired health outcomes, so do the health plan performance. From narrowing the communication gap to enhancing patient care, Hexplora offers an enterprise-grade secured platform to health plans and providers to have complete visibility into performance and utilization metrics, hospitalization rate, ER visits, granular cost data, etc.
Hexplora at a Glance
Hexplora Enterprise Data Warehouse (EDW)
HEX EDW is powered by comprehensive logical and physical data model based on industry-standard design principles. It integrates data across all subject areas and includes a comprehensive data dictionary.
Learn MoreHexplora Population Health Management (PHM)
Collect, analyze and manage specific diseases on population with the Hexplora’s HEX PHM module. It gives you the ability to define multiple attributes thereby improving the effectiveness of the PHM program.
Learn MoreHexplora Quality Analytics
Hexplora’s Quality Analytics module offers 360-degree quality scores down to the member level, integrated workflows to uncover open care gaps and improved quality measure performance.
Learn MoreHexplora Predictive Analysis
Built by leveraging Medicare HCC model, Hexplora’s Predictive Analysis module offers disease identification, stratification, registries, incidence and prevalence trend. Also get risk scores, expenditure forecast, and much more.
Learn MoreHexplora Care Management
Hexplora Care Management module is leveraged by physicians and care managers to deliver optimal clinical outcomes for value-based care management. It manages patient-specific intervention opportunities, Care Gaps, Quality Gaps, and HCC Gaps, etc.
Learn MoreHexplora Provider Engagement
Individually engage physicians to implement provider-specific intervention strategies. Also, get information transparency and visibility into overall healthcare cost and utilization metrics.
Learn MoreWant to know how Hexplora will make a difference to your Health Plans?
Schedule a call with our experts.